Cancer Therapy’s Future: Cell Membrane Coated Nanoparticles
Can nature’s own cell membranes change the way we deliver medicine?
What if medicines could travel through the body like highly trained agents, avoiding every trap set by the immune system, arriving only at their intended destination, and acting with precision? This is not science fiction. It is the promise of a new approach in nanomedicine known as cell membrane coated biomimetic delivery systems, or CMC-BDS.
A recent review titled "Stealth missiles with precision guidance: A novel multifunctional nano-drug delivery system based on biomimetic cell membrane coating technology" explores how scientists are combining natural biology with nanotechnology to solve some of the toughest challenges in drug delivery. By wrapping nanoparticles with real cell membranes, they give these tiny carriers the same surface features and behaviors as the cells they copy. This means they can hide from the immune system, target specific tissues, and cross biological barriers that normally keep drugs out.
The potential applications are wide-ranging. Cancer therapies could become more effective and less toxic. Stroke treatments could reach damaged brain tissue more reliably. Inflammatory diseases could be treated at the source rather than flooding the entire body with medication. The idea is as elegant as it is ambitious: use nature’s own design to make medicine smarter.
Key Highlights
Cell membrane coated biomimetic delivery systems are made by wrapping nanoparticles in natural cell membranes, giving the particles the same properties as the source cells.
They can move through the body without being detected by the immune system, reach diseased tissues with high accuracy, and remain in circulation for longer periods.
Scientists are working with membranes from a variety of sources, including red blood cells, leukocytes, platelets, tumor cells, bacteria, and combinations of different cell types, each offering unique benefits.
The membrane coatings can be further engineered or combined to add more targeting abilities and therapeutic functions beyond the natural properties of the cells.
Researchers have already applied this technology to treat tumors, ischemic stroke, and a range of inflammatory diseases.
This approach solves several problems associated with older synthetic coatings such as polyethylene glycol, which can trigger immune responses after repeated use.
The technology is versatile enough to be used for chemotherapy, gene therapy, phototherapy, and immunotherapy.
Scaling up production, ensuring safety, and gaining regulatory approval remain important challenges before these systems can become common in clinical practice.
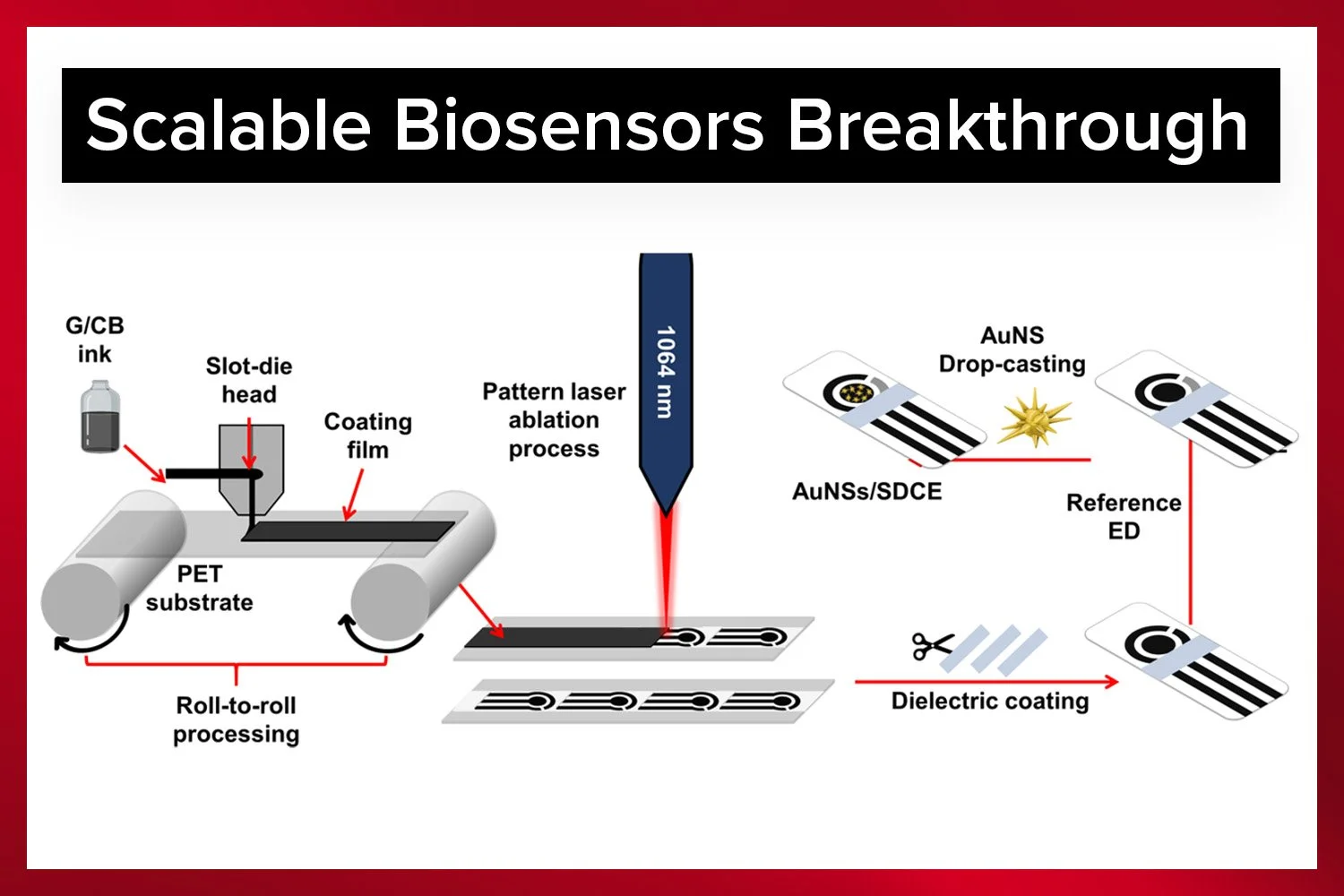
Discover how lab-scale slot-die coating improves pharmaceutical and medical device development through precise, uniform coatings for testing and prototyping.
What is Cell Membrane Coating Technology and Why Does it Matter?
Traditional nanodrug delivery systems already represent a leap forward compared to conventional medicine. They can carry large amounts of drug, protect fragile compounds from breaking down in the body, and release their cargo in controlled ways. Yet they face three stubborn problems:
The immune system quickly identifies and removes them.
They struggle to reach only the desired tissues.
They often cannot cross physical barriers such as the blood–brain barrier.
Cell membrane coating technology offers a solution by literally clothing nanoparticles in the membranes of real cells. A red blood cell membrane, for instance, carries the CD47 protein that tells immune cells “do not eat me.” A platelet membrane can home in on sites of vascular injury. A leukocyte membrane can follow chemical trails to inflamed tissue. When these membranes are carefully extracted and wrapped around a nanoparticle, the result is a carrier that can move through the body as if it belonged there.
This approach also offers unmatched flexibility. Scientists can choose the membrane source based on the disease they want to treat. They can combine membranes from different cells to gain multiple capabilities at once. And they can add extra functions through chemical modification or genetic engineering of the source cells before harvesting their membranes.
The Significance of the Review
This review is not just a summary of past work. It serves as a detailed guide to the current state of the field, explaining both the opportunities and the obstacles. It compares the strengths and weaknesses of membranes from different sources, outlines the main methods for creating the membrane-coated particles, and surveys the growing list of diseases where the technology is being tested.
For scientists and companies interested in advanced delivery systems, this is the kind of map that helps them decide which path to take. For example, someone developing a treatment for brain inflammation might learn that neutrophil membranes can naturally cross into the brain during inflammatory events, making them an ideal coating. Someone working on long-acting cancer drugs might see that red blood cell membranes can extend circulation time dramatically.
Achieve pristine, contamination-free coatings with the Laboratory Roll-to-Roll Coater.
How CMC-BDS Are Made
The process begins with cell membrane extraction. For simple cells like red blood cells or platelets, the membranes are separated from the rest of the cell by placing them in a hypotonic solution that causes them to burst, followed by purification steps to remove internal components. For more complex cells such as immune cells or tumor cells, the process is more involved, requiring physical disruption and careful separation from the cell’s nucleus and other structures.
Next comes nanoparticle core fabrication. This is the heart of the delivery system and can be made from biodegradable polymers, lipids, peptides, proteins, or even inorganic materials like gold or silica. The choice depends on the drug being delivered and the desired release profile.
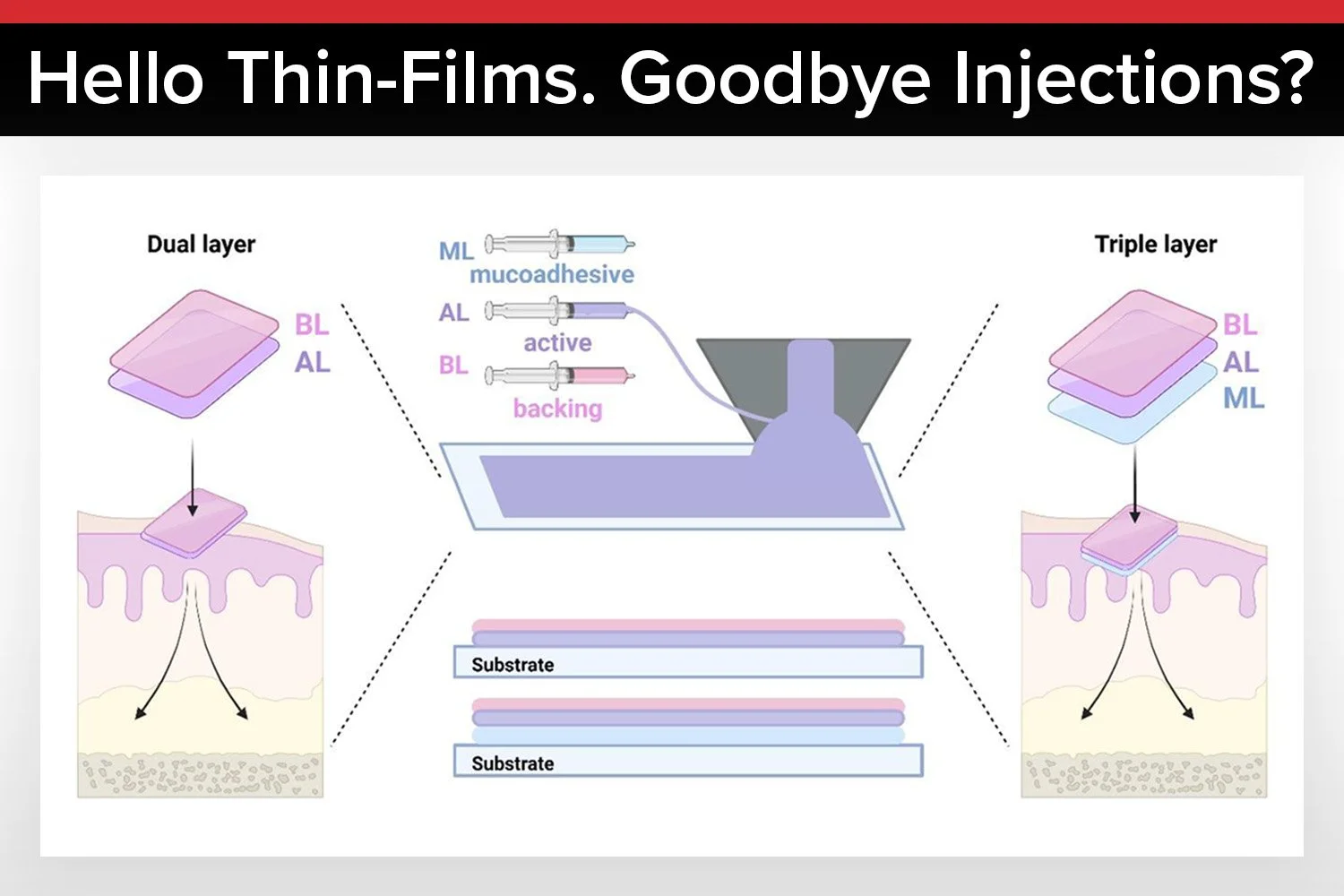
Finally, membrane-core fusion wraps the core with the membrane. This can be done by extrusion, which forces the mixture through tiny pores to form a uniform coating, by sonication, which uses ultrasound to drive the coating process, or by electroporation, which uses short bursts of electricity to fuse the membrane to the core. Each method has tradeoffs in terms of coating quality, preservation of biological activity, and scalability.
Applications in Medicine
Tumor Therapy
Cancer remains one of the most challenging diseases to treat, and nanomedicine has long been seen as a way to improve outcomes. CMC-BDS can help in several ways. In chemotherapy, they can deliver drugs directly to tumor tissue, reducing damage to healthy cells. In gene therapy, they can carry genetic material that disables cancer-promoting genes. In photodynamic therapy, they can carry light-sensitive compounds that, when activated, produce reactive oxygen species to kill cancer cells. In photothermal therapy, they carry agents that heat up under specific light wavelengths to destroy tumors. They can also play a role in immunotherapy, helping the immune system recognize and attack cancer cells more effectively.
Ischemic Stroke
One of the greatest challenges in treating stroke is getting drugs into the brain. The blood–brain barrier blocks most therapies, even when they are desperately needed. CMC-BDS can be coated with membranes from cells that naturally cross this barrier during inflammation, such as neutrophils or macrophages. This allows protective agents, antioxidants, or gene-silencing molecules to reach damaged brain tissue and potentially reduce long-term disability.
Inflammatory Diseases
Inflammation underlies many diseases, from autoimmune conditions to organ damage after injury. CMC-BDS can be coated with immune cell membranes that naturally home in on inflamed tissue. This allows anti-inflammatory drugs to be delivered directly to where they are needed, reducing side effects and improving effectiveness.
Learn the complete process of creating uniform thin films using a slot-die coater.
Future Outlook
The promise of this technology is matched by the challenges it must overcome. Producing these particles in large quantities while maintaining consistent quality is not easy. Safety testing must address concerns about using membranes from cancer cells or bacteria. Personalization will also be important, as the best membrane type and drug combination may vary from patient to patient.
If these issues can be addressed, CMC-BDS could become a standard tool in precision medicine. The idea of a drug delivery system that can disguise itself, navigate the body intelligently, and act only where needed could change the way many diseases are treated.
Conclusion
Cell membrane coated nanoparticles combine the sophistication of biology with the precision of nanotechnology. By mimicking the body’s own cells, they avoid detection, reach their targets, and perform their tasks with minimal collateral damage.
The review makes clear that this is more than an experimental idea. It is already producing promising results in preclinical research for cancer, stroke, and inflammatory diseases. The road to clinical use will require more work, but the direction is set. If successful, CMC-BDS could usher in a new era where medicine moves through the body like a trusted ally rather than an invasive foreign object.
Authors
Yuyan Zhou
Xinyue Wang
Xiaorong Tian
Deyu Zhang
Hanxiao Cui
Wei Du
Zhenghui Yang
Jiayu Li
Wanshun Li
Jiaheng Xu
Ying Duanmu
Ting Yu
Fengping Cai
Wenhao Li
Zhendong Jin
Wencheng Wu
Haojie Huang
Get Professional Support for Your Coating Needs
Need help with slot-die coating, coating machines, or any related applications?
Contact infinityPV’s experts today for professional guidance and support.






















Probably the World’s Most Compact R2R Slot-die Coater: A compact, fully integrated roll-to-roll coating platform for laboratories, complete with a mounting system, anodized rollers, a syringe pump, a 65 mm stainless slot-die head and an infrared oven system—delivering unmatched precision and scalability.